See my earlier posts on IRA worth negotiation on drug choice (Half 1) and producer knowledge submission (Half 2).
At present we’ll speak in regards to the negotiation course of and the way CMS will set the utmost truthful worth (MFP)
How will CMS worth throughout dosages?
“CMS will base the one worth on the price of the chosen
drug per 30-day equal provide (moderately than per unit—reminiscent of pill,
capsule, injection—or per quantity or weight-based metric), weighted throughout
dosage types and strengths.”
Is there a most worth or “ceiling” for the utmost
truthful worth (MFP) that CMS will provide?
The utmost MFP quantity will probably be no larger than:
- An quantity equal to the sum of the plan-specific
enrollment weighted quantities - The decrease of: the common non-FAMP in 2021
elevated by inflation (CPI-U) or the common non-FAMP worth in February 2025
CMS will combination the 60 quantities decided for every NDC-11 for the chosen drug to calculate a single quantity – individually for every methodology – throughout dosage types, strengths, and package deal sizes of the chosen drug. These quantities can then be instantly in contrast, and the ceiling for the one MFP of the chosen drug (together with all dosage types and strengths) would be the decrease quantity.
Pattern packages, NDCs from secondary producers, NDCs
with no amount disbursed or NDCs with gross lined prescription drug prices of
$0 is not going to be included within the MFP calculation.
Can some claims be excluded from the MFP refund?
As soon as the MFP worth is set, there are some instances the place
a producer wouldn’t need to pay the MFP refund. These embody:
“…[justification] codes for the drug being prospectively bought at or under the MFP, the producer and dishing out entity having a individually negotiated refund quantity distinct from the Commonplace Default Refund Quantity, and the declare being excluded from MFP refunds beneath part 1193(d)(1) of the Act”
CMS has to justify the MFP to producers. How will it do that?
The CMS justification will observe a 4-step course of:
- Identification of therapeutic different(s), if any, for the chosen drug. This contains FDA-approved medicine for the related indication and off-label use if included in nationally acknowledged, evidence-based tips and in a CMS-recognized compendia. CMS will start by figuring out therapeutic options throughout the similar pharmacologic class as the chosen drug based mostly on properties reminiscent of chemical class, therapeutic class, or mechanism of motion, after which additionally think about therapeutic options in numerous pharmacologic lessons based mostly on CMS’ overview of related knowledge (see query under).
- Measure the worth of the therapeutic options. For Half D medicine, that is whole gross lined drug price (TGCDC) web of DIR and CGDP funds and/or the Common Gross sales Worth (ASP) for Half B medicine (or prior 12 months MFP if relevant)
- Decide if drug has distinctive profit. Consider whether or not the chosen drug—relative to therapeutic options—addresses an unmet want, has a useful impression on IRA particular populations, and the extent to which the chosen drug represents a therapeutic advance in comparison with therapeutic different(s)
- Additional adjustment of preliminary worth. These changes will probably be based mostly on producer submitted knowledge together with: (1) R&D prices and R&D prices recouped, (2) present unit prices of manufacturing and distribution; (3) prior Federal monetary assist for novel therapeutic discovery and improvement; (4) pending and permitted patent functions or exclusivities; and (5) market knowledge and income and gross sales quantity knowledge for the drug within the US., and (6) non-compulsory producer submitted knowledge.
What knowledge does CMS use to find out therapeutic options?
“…CMS will use knowledge submitted by the Main Producer and the general public, FDA-approved indications, drug classification techniques generally used within the public and industrial sector for formulary improvement, CMS-recognized Half D compendia, broadly accepted scientific tips, the CMS led literature overview, drug or drug class critiques, and peer-reviewed research.”
How may CMS set the preliminary worth provide?
The first manner CMS will set it’s preliminary worth provide for
2027 relies on the web worth of therapeutic options.
Nonetheless…
If the chosen drug has no therapeutic different, if the costs of all therapeutic options recognized are above the statutory ceiling for the MFP…or if there’s a single therapeutic different for the chosen drug and its worth is above the statutory ceiling for the MFP, then CMS will decide the place to begin for the preliminary provide based mostly on the FSS or…“Massive 4 worth”…whichever is decrease. If the FSS and Massive 4 costs are above the statutory ceiling, then CMS will use the statutory ceiling as the place to begin for the preliminary provide.
Why did CMS select to set it’s preliminary worth based mostly on the
worth of therapeutic options?
Word that CMS did think about quite a lot of choices for setting
the preliminary worth provide together with web costs, unit price of manufacturing/distribution,
home references worth to the Federal Provide Schedule (FSS) worth, a “truthful
revenue” worth based mostly on whether or not R&D prices have been recouped and margin on
unit price of manufacturing and distribution, however settled on the web worth of
therapeutic options.
Nonetheless, it argues that the online worth of therapeutic options—regardless of
limitations—is a most well-liked possibility:
“In taking this strategy, CMS acknowledges that the therapeutic different(s) for a particular drug might not be priced to replicate its scientific profit, nonetheless, utilizing Internet Half D Plan Fee and Beneficiary Legal responsibility, ASPs, or MFPs of therapeutic options permits CMS to begin growing the preliminary provide throughout the context of the price and scientific advantage of a number of medicine that deal with the identical illness or situation. By utilizing the worth(s) of the chosen drug’s therapeutic different(s), CMS will be capable to focus the preliminary provide on part 1194(e)(2) components by adjusting this place to begin relative as to whether the chosen drug gives extra, much less, or comparable profit in comparison with its therapeutic different(s).”
What components will impression CMS’s choice to regulate its
preliminary provide?
Some issues embody:
- Scientific profit conferred by the chosen drug
in comparison with its therapeutic different(s), - Influence on patient-reported outcomes and affected person
expertise - Influence on caregivers
- Utilization patterns of the chosen drug versus its
therapeutic different(s) - Suggestions from consultations with clinicians,
sufferers or affected person organizations, tutorial specialists, and/or the FDA - Influence on CMS particular populations (people
with disabilities, the aged, people who’re terminally ailing, kids,
and different Medicare beneficiaries) - Whether or not or not the therapy meets an unmet
medical want
Key related info that will probably be thought-about embody: “…peer-reviewed
analysis, professional experiences or whitepapers, clinician experience, real-world
proof, and affected person expertise.” Key
outcomes of curiosity to be thought-about embody quite a lot of outcomes, together with
patient-centered outcomes, and affected person expertise.
Though CMS notes that it’s going to not use cost-effectiveness
evaluation based mostly on QALYs, it has not dominated on whether or not it might probably use different
approaches reminiscent of equal worth of life years gained (evLYG), well being years in
whole (HYT) or generalized and risk-adjusted QALYs (GRA-QALYs).
These components will impression the worth via a qualitative choice
course of.
Will caregiver expertise impression CMS selections?
Sure. The
steerage says that “CMS might also think about the caregiver perspective to the
extent that it displays instantly upon the expertise or related outcomes of
the affected person taking the chosen drug.”
Does CMS think about price when evaluating if a therapy is
a therapeutic advance?
Sure.
“CMS will decide the extent to which a particular drug represents a therapeutic advance as in comparison with its therapeutic different(s) by analyzing enhancements in outcomes in comparison with its therapeutic different(s) (e.g., chosen drug is healing versus a therapeutic different that delays development) and can think about the prices of such therapeutic different(s). CMS might think about a particular drug to symbolize a therapeutic advance if proof signifies that the chosen drug represents a considerable enchancment in outcomes in comparison with the chosen drug’s therapeutic different(s) for a sign(s).”
How will the negotiation course of work?
That is summarized within the graphic under.
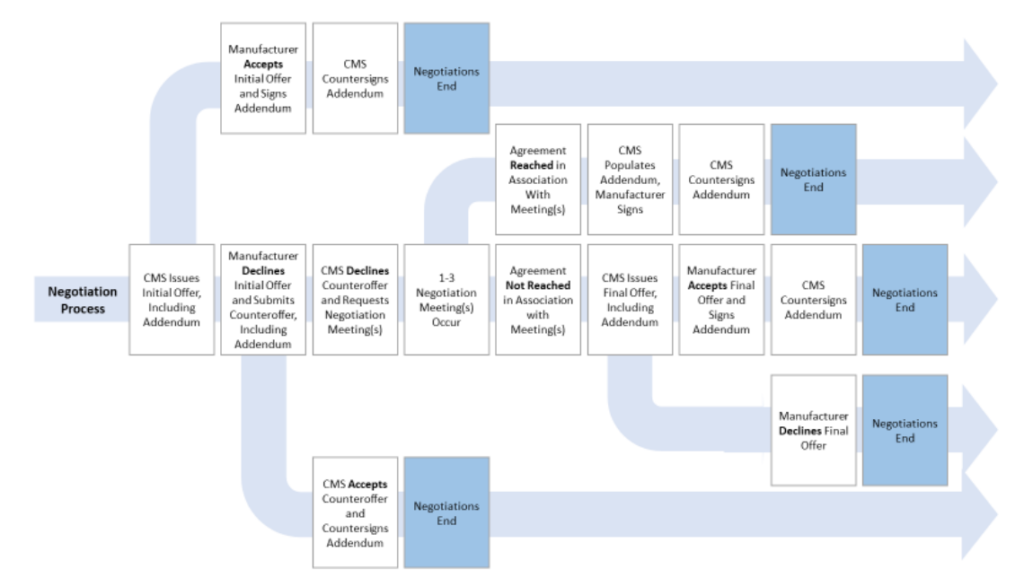
Extra element will be discovered within the CMS steerage doc right here.

